COVID-19 and communities of color: What the data tells us
The novel coronavirus is anything but “a great equalizer.” As the outbreak has progressed through the United States, black and brown communities are facing particularly extreme impacts. New data from the Centers for Disease Control released on April 17 found that while black people make up 13% of the U.S. population, they’re currently accounting for 30% of reported COVID-19 cases. People from Latinx communities are also seeing higher rates of infection and hospitalization.
We’re seeing right now that COVID-19 is disproportionately affecting communities of color—and to understand just how much, and how we can address these disparities, we need data. At Tableau, we are data people. And as the pandemic progresses, we’re seeing just how critical data is to understanding and taking action against it. We’re sharing stories of how data is informing decision-making at the macro level with state governments, and at the local level in small school districts. We’ve seen how data is illuminating the link between COVID-19 and the environment, and how data is enabling leaders to ensure that people’s basic needs, like food and shelter, are still being met.
Our partners at Kaiser Family Foundation are showing just how critical data is and will be for assessing COVID-19’s impacts on communities of color. “With a pandemic, yes, the broad public is at risk,” says Samantha Artiga, Director of the Disparities Policy Project at. “But what we're really seeing with COVID-19 is the strong exposure of all the disparities that individuals and groups have been facing prior to the pandemic.”
COVID-19 is not an equalizer—it’s a force multiplier for pre-existing inequalities. KFF has compiled data on those inequities to help explain some of the disparate impacts we’re seeing across communities, but there’s not enough of it, Artiga says. States and the federal government have only recently started collecting and sharing disaggregated data by race—and they need to do more as the virus progresses so we can truly understand its impacts. Having a clear picture of the data will enable policymakers to craft strategies to mitigate both the immediate and systemic effects of the virus.
Learn more about Tableau Foundation’s work on the issue of equity.
What the data is telling us
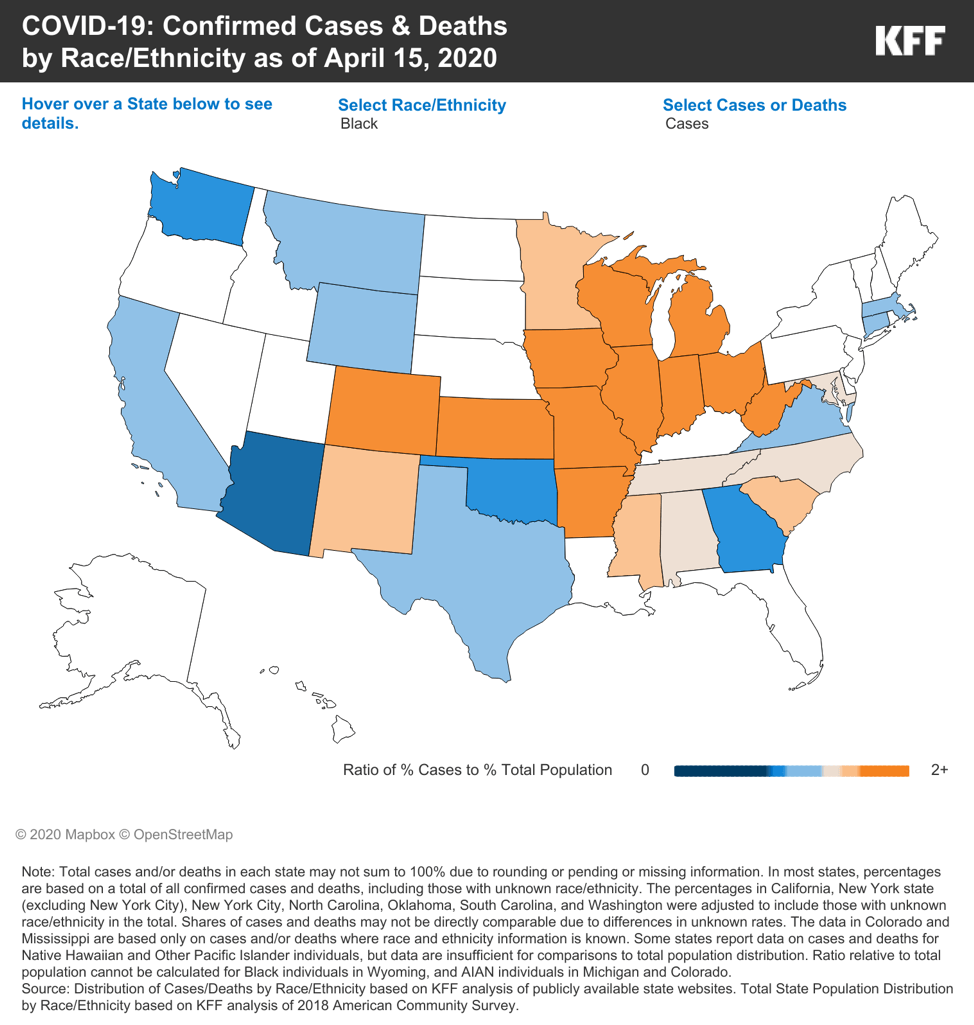
As the COVID-19 outbreak has progressed, it’s only become clearer that people of color are bearing a disproportionate amount of the virus’ burden. The data on race and ethnicity and the novel coronavirus is still very incomplete, Artiga says, but even what we have now is showing a clear picture. Early data from states that are reporting disaggregated data reflects the fact that in many places, black people account for a greater percentage of COVID-19 cases than they do a portion of the population.
According to KFF, “In the majority of states reporting data, Black people accounted for a higher share of confirmed cases (in 20 of 31 states) and deaths (in 19 of 24 states) compared to their share of the total population. These disparities were particularly large in Wisconsin, where Black people made up a four-times higher share of confirmed cases (25% vs. 6%) and an over six-times higher share of deaths (39% vs. 6%) compared to their share of the total population.” KFF also found disparities in a handful of states around the disproportionate burdens faced by Hispanic and Asian communities, and noted that more data is needed to assess the impacts on smaller vulnerable groups, including people who are American Indian or Alaska Native and Native Hawaiian or Other Pacific Islander.
Data from Pew shows a different view of inequities by race: According to the polling company, black and Latinx people are far more likely than white people in the U.S. to view the coronavirus as a threat to their health and communities. The reasons for this disparity in sentiment across race may have to do with the pre-existing inequities that KFF has documented.
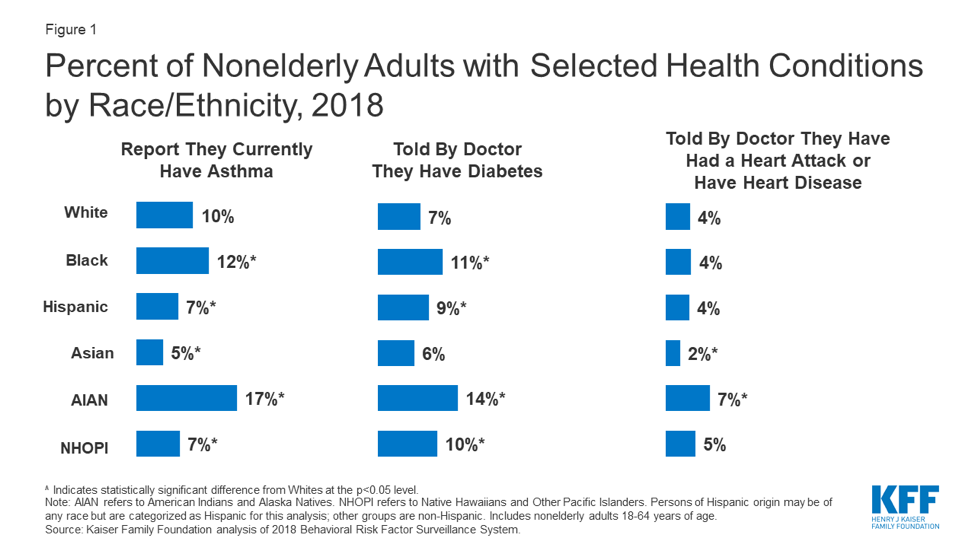
The uneven distribution of health risks
Good health and healthcare are not evenly distributed across the U.S. population. Communities of color face higher risks of experiencing serious symptoms or dying due to COVID-19 because of a greater prevalence of underlying health conditions: diabetes, heart disease, asthma, and lung disease. KFF data shows that black Americans and American Indians and Alaska Natives are more likely than white Americans to report pre-existing health concerns that would heighten their risk amid the coronavirus pandemic. These disparities are not an accident, Keeanga-Yamahtta Taylor recently wrote in The New Yorker: They stem from decades of persistent racial and ethnic discrimination that has fenced communities of color off from good access to care, and the resources that form the foundation of good health.
KFF’s analysis finds that people of color in the U.S. are much more likely to be uninsured than their white counterparts, which creates barriers in accessing care. Beyond the healthcare system, communities of color often face inequities when it comes to necessities like nutrition and access to green space. “Things like access to healthy food, what your transportation options are, what your housing situation is, what your neighborhood and built environment is—all these factors influence an individual's health, and that is applicable to health more broadly as well as the impact of COVID-19,” she says.
Economic vulnerabilities are health vulnerabilities
What underlies these health disparities across demographics is people’s overall economic well-being—which in the United States, is often correlated with race and ethnicity. Black, Latinx, and American Indian and Alaska Native people are much more likely to report income below the poverty line, according to KFF data.
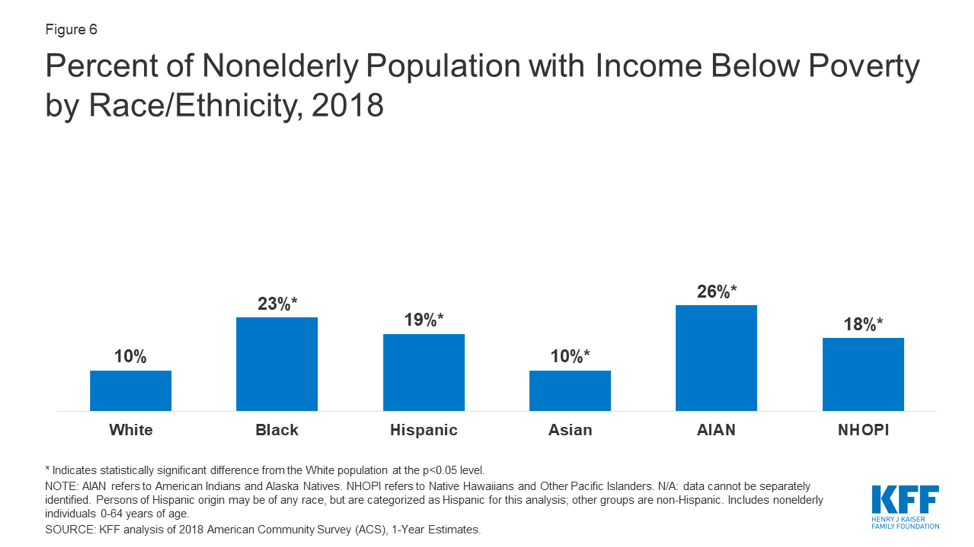
Artiga notes that as a result, “people of color are likely less able to be able to weather or deal with income decreases that may stem from job losses or reduction in work associated with the pandemic—and at the same time, they’re more likely to work in occupations that cannot be done remotely, like grocery store clerks or delivery drivers, which leaves them at higher risk for exposure to the virus.” That’s certainly holding true in Chicago, where Dr. Monica Peek, an associate professor at UChicago Medicine, says that “72% of our deaths here in Chicago residents have been in black Chicagoans. Though again, black Chicagoans just make up 30% of the city's population. The big picture is that racial or ethnic minorities in this city are more likely to be exposed to the virus because they are the ones that are working in jobs that allow the rest of the city to safely stay at home and shelter in place.”
Economic insecurity also affects people’s housing circumstances, which according to The Brookings Institution are a key contributor to the spread of the coronavirus and its inequitable effects. Black majority neighborhoods have much higher concentrations of multigenerational households, and the increased number of people living in close proximity gives the virus more opportunities to spread. Across the U.S., communities of color—especially in urban environments—people are often forced to live in more cramped circumstances due to housing affordability and long-term economic inequities. KFF’s analysis finds that “roughly four in ten Blacks (41%), Hispanics (38%), and Asians (38%) indicate that the area surrounding their residence includes multi-unit residential buildings compared to 23% of Whites.”
As Brookings notes: “The coronavirus does not discriminate, but our housing, economic, and health care policies do. Environmental racism, unaffordable housing, a lack of job opportunities, poverty, and inadequate health care are underlying social conditions, strongly influenced by policy, which place [people of color] and their neighborhoods at risk.”
How policy solutions can avoid perpetuating inequities
To address the underlying conditions exacerbating risk for COVID-19, we need policies informed by the data we have on these inequities to craft policies to address them. States need to continue to ramp up the collection and reporting of data disaggregated by race on both the health impacts of COVID-19 and the economic effects.
“Hopefully, the increased recognition of these disparate impacts can be used as an opportunity for continued focus on addressing disparities moving forward,” Artiga says. “That might look like understanding better where more aid and response is needed—is it in certain areas? Among certain communities? What types of language services need to be made available, and what types of messengers can best reach out to deliver information and connect with communities that are being impacted?”
To reach this understanding—and to develop responses both in the near and long term—policymakers need to begin working now to ensure that the people most disproportionately affected by COVID-19 are directly involved in the decision-making process. “There’s an immediate need for the data to show us who are the communities and people most heavily impacted by COVID-19,” says Dr. Scott Cook of UChicago Medicine, whose research focuses on improving the health and wellness of racial, ethnic, sexual, and gender minority populations in both rural and urban communities. “That will inform not only how we direct resources but—and this isn’t thought about as much—who we bring to the table when we’re developing policies and programs and solutions for the outcomes of this pandemic.”
These populations who are being most impacted during this outbreak, Cook says, “are those who have less power, and have less access to those who are in power.” But the people most affected have insights that others do not about what solutions will be most effective, and what resources are most necessary. Ensuring that the data is used to include them—from the very beginning—in the response process will ensure that the solutions are as effective as they can be, and that they directly address pre-existing inequities, rather than perpetuating them.
関連ストーリー
Subscribe to our blog
Tableau の最新情報をメールでお知らせします